Evaluating Vagus Nerve Stimulation For Migraine Management: A Comprehensive Review
Evaluating Vagus Nerve Stimulation For Migraine Management_ A Comprehensive Review - Seher Deo
ABSTRACT
Background: Vagus nerve stimulation (VNS) changes the function of cranial nerves by placing a small device in the body that sends electrical signals via the vagus nerve to the neck and brain stem. These signals alter pain responses from the brain, in turn helping with migraine management.
Objective: This paper looked at whether vagus nerve stimulation is an effective treatment for migraines.
Methods: Articles were searched via PubMed with the key terms “vagus nerve stimulation,” “migraine,” and “pain relief.” All studies included were original research articles, had human participants, and were published in English. Studies were excluded if they were review articles, involved non-human subjects, or were published in any language other than English.
Results: VNS is an effective treatment for migraines. It reduces attack frequency, pain intensity, and medication dependency.
Conclusion: To treat migraines, VNS can be used as an alternative to medications. It helps reduce the risk of medication overuse headaches (MOH), as well as other medication side effects such as compulsive medication use, and behavioral problems.
INTRODUCTION
Migraines are ranked as the third most common neurological condition in the world [1]. This disorder is highly prevalent, and remains among the top three from ages 5 to 80 [1]. It is common among people of all ages, genders, and races, making it a universal burden [1]. Fifty percent of migraine patients self-treat their headaches, often leading to heavy reliance on medications such as analgesics and anti-emetics [1]. While taking medications as treatment is not inherently wrong, there are many health risks associated with it [1]. Medication overuse has been known to cause addiction, compulsive medication use, and behavioral problems [3]. It can also lead to medication-overuse headache (MOH), which is a common neurological disorder [3]. MOH often turns episodic headaches into chronic headache disorders, leading to severe suffering and disability [3]. Both migraines and MOH have critical effects on quality of life [1]. Recurrent attacks disrupt family dynamics, social activities, and occupational performance [1]. Furthermore, people with migraine disorders have higher rates of depression and anxiety compared to those without the condition [1]. Given these widespread personal, social, and clinical consequences, there is a growing need for effective non-pharmacological treatment options. In light of new treatments, vagus nerve stimulation (VNS) is currently being explored as a tool for migraine symptom relief [2]. During VNS, electrical signals are sent via the vagus nerve, which carries those messages up to the brain [2]. Consequently, a network of vagus nerve pathways is activated, connecting the brainstem with various brain regions [2]. In response to signals from the vagus nerve, brain regions implicated in migraines are brought to a more parasympathetic state, reducing pain [2]. VNS is an important alternative to medication use, as it mitigates the health risks of standard medicines and ensures a safer treatment for patients [2,3]. This review paper aims to evaluate the effects of VNS on migraines, either as a standalone intervention or in comparison with a sham treatment.
METHODS
A literature search was conducted in PubMed to identify clinical studies exploring VNS as a migraine treatment. The search strategy combined the following keywords: “vagus nerve stimulation,” “migraine,” and “pain relief.” All studies included were original research articles, had human participants, and were published in English. Studies were excluded if they were review articles, involved non-human subjects, or were published in any language other than English.
RESULTS
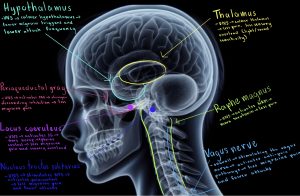
Each of the studies shown in Table 1 published similar results regarding the effectiveness of vagus nerve stimulation in migraine pain relief, reduced headache days, decreased need for rescue medications, and altered connectivity of brain regions [4-8]. Study one looked at how transcutaneous auricular vagus nerve stimulation (taVNS) compares to a sham treatment [4]. The group of taVNS patients had significantly fewer migraine attack days than the sham group, and during these days, their pain intensity was noticeably lower [4]. Furthermore, taVNS increased connectivity between the anterior cingulate cortex, medial prefrontal cortex, and motor-related thalamus subregion [4]. It also decreased the connectivity between the postcentral gyrus, precuneus, and the occipital cortex-related thalamus subregion [4]. These connectivity changes altered sensory processing pathways, which led to pain relief in the taVNS patients [4]. Study two emphasized how the nucleus tractus solitarius, locus coeruleus, periaqueductal grey, raphe magnus, thalamus, and hypothalamus all activate a neural pathway, as shown in Figure 1 [5]. This pathway reduced pain and migraine frequency [5]. It also explored the results of nVNS treatment compared to a sham treatment [5]. The primary outcomes of this study were reduced migraine attack days and pain-free status within 30 min of nVNS use [5]. Two of the six trials in this study saw a decrease in migraine attack days in 4 weeks, and one trial saw a decrease in migraine attacks per week [5]. Secondary outcomes included the status of pain relief at 30 and 60 min, use of rescue medication, satisfaction, adverse events, and pain-free status in ≥50% of treated migraines [5]. The number of patients who reached pain-free status for at least 50% of treated headaches was much higher in the nVNS group compared to the sham group (OR: 2.15; 95% CI: 1.27–3.66; p=0.005) [5]. Study three found that following non-invasive vagus nerve stimulation (nVNS) treatment, 27 of 48 patients (56.3%) felt pain relief at 1 hour, and 17 of these patients (35.4%) were pain-free [6]. At 2 hours, 31 of 48 (64.6%) patients felt pain relief, and 19 of these patients (39.6%) were pain-free [6]. In study four, which compared the results of a nVNS device to those of a sham device, three main periods were looked at: the double-blind, observational, and open-label [7]. During the double-blind period of this study, at 60 minutes post-treatment, 16.3% of the nVNS group’s migraines were pain-free, and at 120 minutes, 22.9% of attacks were pain-free [7]. For the sham group, the pain-free results were 8.6% at 60 minutes and 14.8% at 120 minutes [7]. For all migraines, the nVNS group’s mean decrease in pain score at 60 minutes (0.42) was significantly larger than that of the sham group’s (0.22) [7]. During the observational period, pain-free and pain-relief results were ≥75% at 24 hours and ≥58% at 48 hours for both the nVNS and sham group [7]. During the open-label period, at 120 minutes 23.3% of all attacks were pain-free and 38.1% of them saw pain relief [7]. Altogether, the study found that the group of nVNS patients had a higher percent of pain-free status at 60 minutes (p=0.005) and at 120 minutes (p=0.0026) than the sham treatment group [7]. Lastly, study five observed a similar situation to studies two and four when comparing nVNS treatment to sham treatment [8]. After 30 minutes post-treatment, the percentage of nVNS patients who reported at least a 1-point decrease in pain score was 32.2%, whereas for the sham patients it was 18.5% [8]. At 60 minutes these percentages were 38.8% and 24.0%, and at 120 minutes they were 46.8% and 26.2% [8]. The percentage of nVNS patients that did not need rescue medications was 59.3% after the first attack, and 52.3% for all attacks [8]. For the sham group, these percentages were 41.9% after the first attack and 37.3% for all attacks [8]. Overall, each of these studies consistently revealed that vagus nerve stimulation was effective in relieving migraine pain, lowering the number of headache days, reducing the use of rescue medications, and modifying brain connectivity [4-8].
Table 1. Summary of Results
Author(s), year, title | Aim of study | Study setting, participants, details | Methods including study design | Results |
Zhang et al. (2020) “Transcutaneous auricular vagus nerve stimulation (taVNS) for migraine: an fMRI study.” [4] | To investigate how taVNS affects thalamocortical (TC) circuits and the development of migraines.
Also to explore connection between taVNS and resting state functional connectivity rsFC of the TC network to understand if it eases symptoms of migraine attacks. | Setting: 70 episodic migraineurs from the Second Affiliated Hospital of Guangzhou University of Chinese Medicine. Period: Between May 2017 and May 2019. Age: 18-45 years. Details: Patients randomly selected to receive taVNS or a sham treatment. They use headache diaries to record onset time, duration, pain intensity (measured by VAS score), accompanying symptoms, and rescue medication usage. | This study compared rsFC before and after 4 weeks of taVNS treatment of migraines without aura and compared this with a sham taVNS device. The taVNS was applied to the left cymba concha, whereas the sham was applied to the left tail of the helix using electronic acupuncture. | Of the 35 taVNS patients and 35 sham taVNS, 59 (33taVNS and 26 sham) completed the 2 fMRI scans, and the remaining 11 did not because of various reasons.
The taVNS group had much fewer migraine attack days and less pain intensity compared to the sham taVNS group. |
Lai et al. (2019) “Cervical Noninvasive Vagus Nerve Stimulation for Migraine and Cluster Headache: A Systematic Review and Meta-Analysis.” [5] | To compare the effects of cervical nVNS treatment with sham-device treatment/standard care on headache days, pain-free status, abortive medication use, etc.
Also to study how central nervous system functions are affected during vagus nerve stimulation. | Setting: 983 patients from 6 trials. Details: The patients had a diagnosis of primary headache disorders. They were randomly assigned cervical nVNS treatment or a sham treatment. The nVNS treatment consisted of a low-voltage electrical signal that took place for 1 ms and repeated every 40 ms. It had a maximum output current of 60 mA and 24 V.
| This study compared the pain intensity and number of pain free days between the two study groups. Pain was recorded on a 4-point scale.
The pain-free status in at least 50% of treated headaches meant that patients had pain scores of 0 during the assessment in at least 50% of their treated headaches. | reduced migraine attack days and pain-free status within 30 min of nVNS use. 2of the trials saw a decrease in attack days in 4 weeks, and 1 trial saw a decrease in headaches per week.
The percentage of patients who reached pain-free status in at least 50% of treated headaches was much higher in the nVNS group compared to the sham group. |
Barbanti et al. (2015) “Non-invasive vagus nerve stimulation for acute treatment of high-frequency and chronic migraine: an open-label study.” [6] | To analyze the impact of nVNS on migraine attacks at 1 and 2 hours on patients who suffer from chronic migraines (CM) 15 days or more in a month and high-frequency episodic migraines (HFEM) 8 days or more in a month. | Setting: Headache Center of Carlo Besta Neurological Institute Foundation in Milan and the Headache and Pain Unit of the IRCCS Sam Raffael Pisana in Rome, Italy Period: February 1-October 1 2013. Age: 50 patients, ages 18-65 (female/male:40/10) Details: Neurologists, counselors, and 3-6 patients took part in monthly educational meetings. Patients were instructed to self-treat up to three consecutive migraines using nVNS. | Within 20 minutes of the onset of each migraine, patients delivered two 120-s doses of electrical stimulation every 3 minutes to the right cervical branch of the vagus nerve. Pain level was measured using a 0 to 10 visual analog scale (VAS). Pain measurements were taken at 1 and 2 hours post nVNS treatment.
VAS score of 0 meant pain-free and pain relief was determined by at least a 50% reduction in VAS score. | Of the total 50 patients, 48 patients treated 131 migraines total, and 2 patients did not treat any.
For all 131 migraines at 1 hour pain relief was 50 of 131 (38.2%). At 2 hours it was 67 of 131 (51.1%). Pain free status at 1 hour was 23 of 131 migraines (17.6%). At 2 hours it was 30 of 131(22.9%). |
Martelletti et al. (2018) “Consistent effects of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: additional findings from the randomized, sham-controlled, double-blind PRESTO trial.” [7]. | To prove that nVNS increases the chances that a migraineur experiences mild pain or pain free status 2 hours post treatment. | Setting: Multicenter, randomized, double-blind, sham-controlled PRESTO trial. Period: January 11, 2016 to March 31, 2017. Age: 248 patients between 18 and 75 years. Details: Patients <50 old when their migraines began, and have had <15 headache days in a month for the last 6 months, and have 3-8 attacks monthly. | 122 patients randomly assigned to nVNS and126 to sham treatment. Within 20 minutes of migraine onset, patients gave themselves 120-s stimulations to the right and left sides of the neck. They wrote down post treatment stats in diaries for 15, 30, 60, and 120 minutes as well as 24 and 48 hours. | Out of 243 patients, 239 participated in the open-label period (nVNS n=117, sham n=122).
Of these 239, 238 (>99%) completed this period of the study, and 220 (92%) treated at least 1 attack. The group of nVNS patients had a higher percent of pain free status at 60 (p=0.005) min and 120 (p=0.0026) min compared to the sham treatment group. |
Grazzi et al. (2018) “Practical and clinical utility of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: a post hoc analysis of the randomized, sham-controlled, double-blind PRESTO trial.” [8]. | To use PRospectivE Study of nVNS for the acute Treatment Of migraine (PRESTO) to evaluate the effectiveness of nVNS compared to a sham treatment, including impact on need for rescue medication and pain level.
| Setting: Study performed at 10 Italian sites. Period: January 11, 2016 through March 31, 2017. Age: 285 patients, 18-75 years. Details: Patients <50 years when their migraines started, and needed to have a frequency of 3-8 migraines monthly. Of the total 285 patients, 248were randomly assigned nVNS treatment (n=122) and sham treatment (n=126). Pain was measured on a 4-point scale. | Within 20 min of the beginning of a migraine, patients gave themselves 120-s stimulations to the left cervical branch of the vagus nerve, to be repeated if pain did not subside after 15 min. At 120 min, this could be optionally repeated or they could resort to rescue medications. The percentage of migraineurs with at least a 1-point reduction in pain score on the 4-point scale was measured at 30, 60, and 120 min following the 1st attacks. | More nVNS group patients than sham patients performed treatment when their migraines were severe (1st attack: nVNS=23.5%, sham=15.1%; all attacks: nVNS=25.1%, sham=17.6%).
Patients in the nVNS group with a significantly higher than 1-point decrease at 60 min were 33.3%, and the sham patients for this were 22.2%. At 120 min it was nVNS=39.4% and sham=26.4%. |
Figure 1. Diagram of various brain regions affected by VNS.
DISCUSSION
Each of the five studies found that vagus nerve stimulation (VNS) is an effective treatment for migraine pain and reduces the frequency of attacks [4-8]. Specifically, VNS delivers electrical signals to the vagus nerve, which transmits these messages to the brain [2].The stimulation engages a network of neural pathways that connect the brainstem to multiple regions of the brain [2]. Consequently, brain plasticity is increased, and a parasympathetic state is promoted, helping to alleviate pain [2]. One of the ways VNS efficiency was tested was by comparing it to a sham treatment [4-5,7-8]. Each of the studies that conducted this experiment found that VNS was significantly more effective than the sham treatment in easing migraine pain and, at times, relieving the pain altogether [4-5,7-8]. Furthermore, the studies showed that VNS patients experienced notably fewer attack days than those who received the sham treatment [4-5]. The consistently strong performance of VNS throughout these studies emphasizes that it is a reliable and functional treatment for migraines [4-5]. Given the high world-wide prevalence of migraines, it is imperative that new and effective treatments for migraines are explored [1]. Each of the studies was conducted in varying parts of the world, allowing for a diverse ethnic demographic of patients [4-8]. Study one was conducted in the Second Affiliated Hospital of Guangzhou University of Chinese Medicine [4]. Study two was held in the Taipei Medical University of Taiwan [5]. Study three took place in the Headache Center of the Carlo Besta Neurological Institute Foundation in Milan and the Headache and Pain Unit of the IRCCS San Raffaele Pisana in Rome, Italy [6]. Lastly, the fourth and fifth studies were conducted across ten Italian sites, whose details are not specified in the articles [7,8]. The diversity of these locations adds to the depth of these studies, further supporting the effectiveness of VNS [4-8]. All participants were aged 18 to 75 years, and while this range is relatively wide, none of the patients were minors [4-8]. This is important to note because migraines affect many young people, often beginning during puberty [1]. Future VNS studies should include patients of younger ages to see how the treatment impacts developing physiology. Overall, VNS is an impactful treatment for migraines, and the knowledge gained from future studies will continue to strengthen its effectiveness [4-8].
References
- Migraine and other headache disorders. World Health Organization. Accessed November 28, 2025. https://www.who.int/news-room/fact-sheets/detail/headache-disorders.
- Austelle CW, Cox SS, Wills KE, Badran BW. Vagus nerve stimulation (VNS): recent advances and future directions. Clin Auton Res. 2024;34(6):529-547. doi:10.1007/s10286-024-01065-w
- Fischer MA, Jan A. Medication-Overuse Headache. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 22, 2023.
- Zhang Y, Huang Y, Li H, et al. Transcutaneous auricular vagus nerve stimulation (taVNS) for migraine: an fMRI study. Reg Anesth Pain Med. 2021;46(2):145-150. doi:10.1136/rapm-2020-102088
- Lai YH, Huang YC, Huang LT, Chen RM, Chen C. Cervical Noninvasive Vagus Nerve Stimulation for Migraine and Cluster Headache: A Systematic Review and Meta-Analysis. Neuromodulation. 2020;23(6):721-731. doi:10.1111/ner.13122
- Barbanti P, Grazzi L, Egeo G, Padovan AM, Liebler E, Bussone G. Non-invasive vagus nerve stimulation for acute treatment of high-frequency and chronic migraine: an open-label study. J Headache Pain. 2015;16:61. doi:10.1186/s10194-015-0542-4
- Martelletti P, Barbanti P, Grazzi L, et al. Consistent effects of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: additional findings from the randomized, sham-controlled, double-blind PRESTO trial. J Headache Pain. 2018;19(1):101. Published 2018 Nov 1. doi:10.1186/s10194-018-0929-0
- Grazzi L, Tassorelli C, de Tommaso M, et al. Practical and clinical utility of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: a post hoc analysis of the randomized, sham-controlled, double-blind PRESTO trial. J Headache Pain. 2018;19(1):98. Published 2018 Oct 19. doi:10.1186/s10194-018-0928-1



